Hypertension
High blood pressure, also known as hypertension, is a common and important condition in which the force of blood against the artery walls is too high. There are typically no symptoms, however, blood pressure directly influences cardiovascular health. Over 100 million Americans have high blood pressure and, among non-pregnant adults, treatment for those with a diagnosis of hypertension is the most common reason for office visits and the chronic use of prescription medicines. Hypertension is the top risk factor in the US, with 454,347 attributed deaths in 2017.

Diagnosis
-
The identification of hypertension is complex because blood pressure has high variation for every individual. It requires integration of repeated blood pressure measurements, using proper technique (see this video), both in and out of a physician’s office, in order to address “white coat” and “masked” hypertension phenomena. At least 12 to 14 measurements should be obtained at home and at various times of the day, on both arms, and over a period of one week.
-
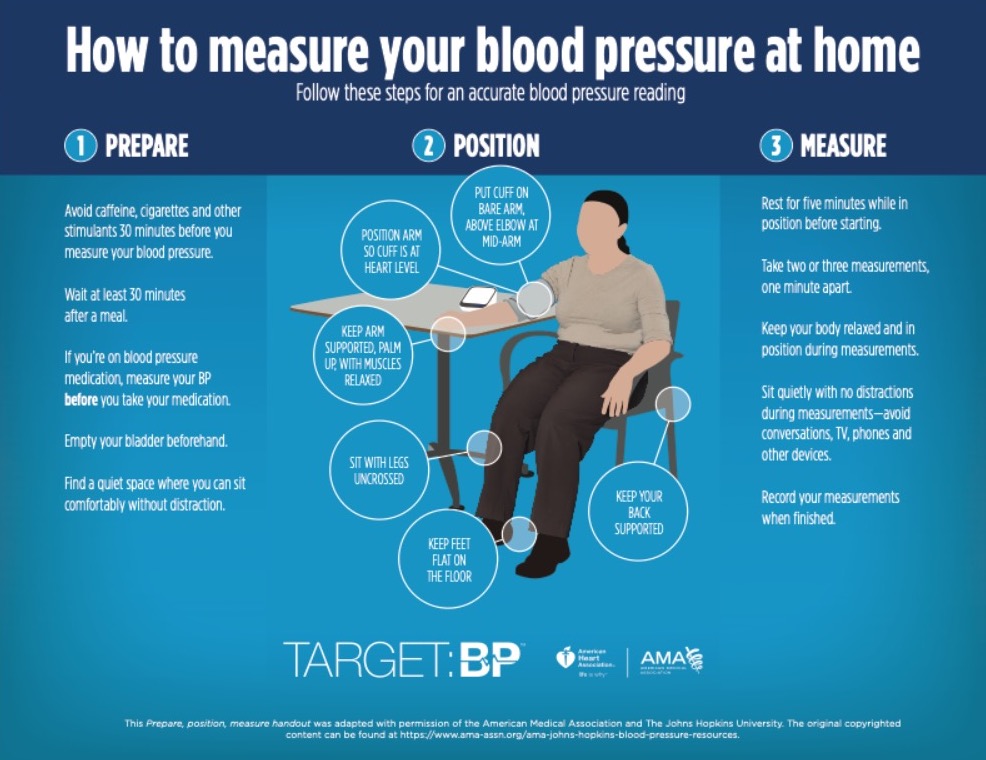
Twenty-four-hour ambulatory blood pressure monitoring (“ABPM”) is the “gold standard” for confirming a diagnosis of high blood pressure (“primary hypertension”), especially if there are differences between readings in and out of a physician’s office. Home blood pressure measurements should be based on the instructions in this chart.
-
If blood pressure is determined to be elevated through a series of proper measurements, further tests should be performed to evaluate potential for cardiovascular risk and risk to other organs.
-
According to the American Dental Association, a dental visit is an important opportunity to measure and identify potential hypertension, for further follow-up with primary care physician, given (1) interactions between dental treatments (like medications and local anesthesia) and hypertension and (2) the prevalence of hypertension among dental patients.
-
Any particular threshold of appropriate blood pressure is relatively weak, since the relationship between blood pressure and cardiovascular risk is graded and continuous without an obvious inflection point. There are several sets of published measurement guidelines; these guidelines are generally useful for screening. However, even a single reading of significantly elevated blood pressure, defined as systolic pressure >= 180 and/or diastolic pressure >= 120 mmHg, does require urgent evaluation by a medical professional.
-
While it is commonly stated that blood pressure must be taken by a doctor or nurse in order to identify hypertension, the opposite is true. Measurement of blood pressure exclusively in a physician’s office has been shown, in randomized control trials, to be an inferior predictor of cardiovascular risk as compared with self-monitoring.
Causes
-
Primary, or essential, hypertension makes up 90 to 95% of all hypertensive cases and arises from specific risks. The risk factors that are strongly and independently associated with development of high blood pressure include age; obesity; family history (genetic factors account for approximately 30 percent of variation in blood pressure); race; reduced nephron number (related to kidney function); high-sodium diet (i.e., above 3g per day); excessive alcohol consumption (i.e., 6 or more drinks per day); and physical inactivity.
-
Secondary hypertension affects 5 to 10% of those diagnosed with hypertension and has a medically described cause, such as vascular disease or hormonal dysfunction.
-
Other risk factors include medications such as oral contraceptives with higher doses of estrogen, chronic use of ibuprofen and acetaminophen, and antidepressants.
-
Hypertension and obstructive sleep apnea (“OSA”) frequently co-exist. There is some, but not consistent, evidence that OSA is a cause of hypertension.
-
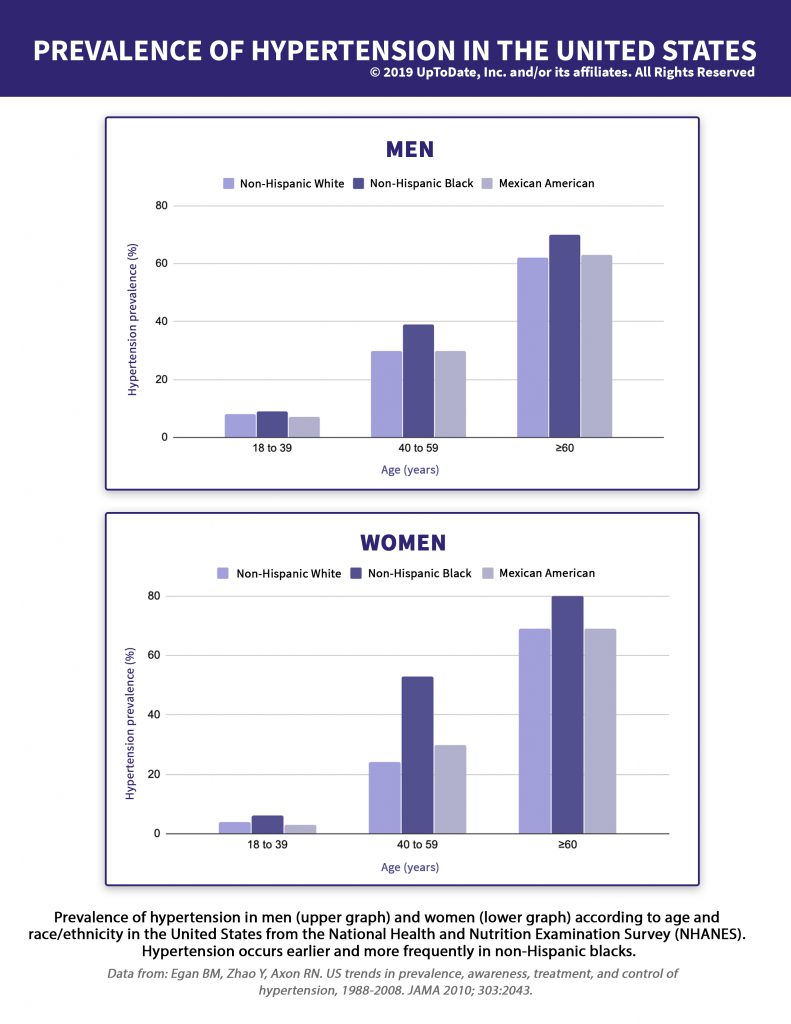
While many believe that men are more at risk of hypertension and other heart problems, this is not true. In fact, gender is not a risk factor as hypertension affects both men and women equally, although at different ages and with different racial impacts as shown in this chart.
“ I Heard That…
-
Strength training helps to lower high blood pressure. Is that true?
 Yes!
Yes! See this study from the American Heart Association. And, even transcendental meditation, as you see in this piece from the American Heart Association.
-
You can measure your blood pressure on your wrist! Is that true?
 Yes; there is currently at least one FDA-approved device to do.
Yes; there is currently at least one FDA-approved device to do. It has more than 80 patents filed; see CNET’s coverage of the Omron watch.
Treatment
-
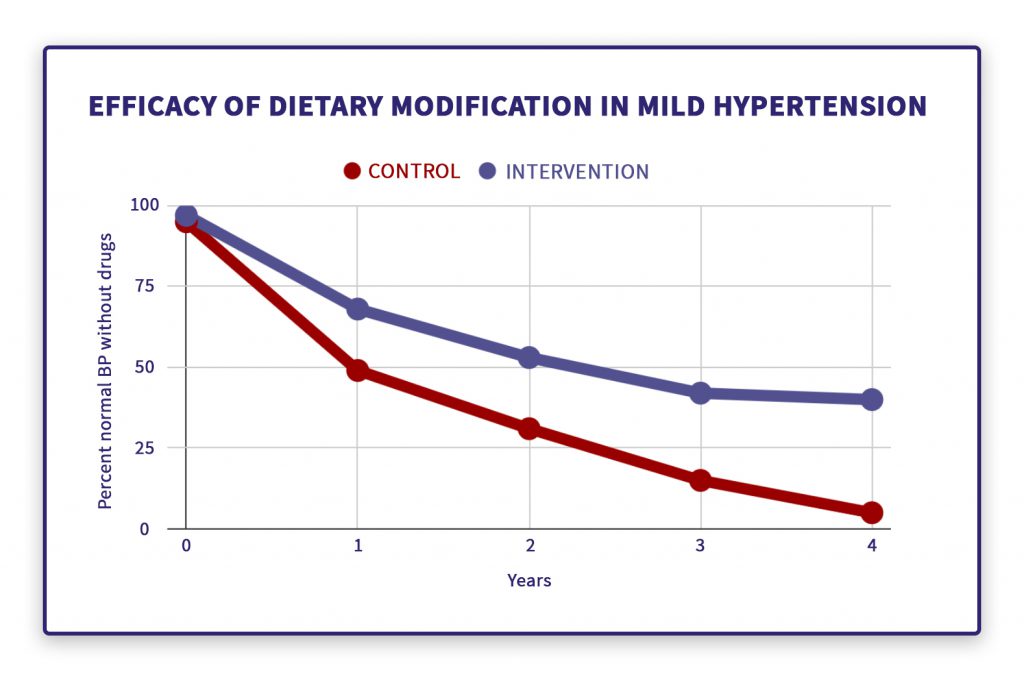
The enduring treatment for hypertension is lifestyle modification, which includes dietary salt reduction, potassium supplementation, weight loss, DASH diet, exercise and limited alcohol intake. As shown in this chart, over several years after removal of medication, hypertension recurred in 90% of individuals with no dietary modification (“control”) but only 60% of individuals with a combined intervention of weight loss, salt restriction, and avoidance of excessive alcohol.
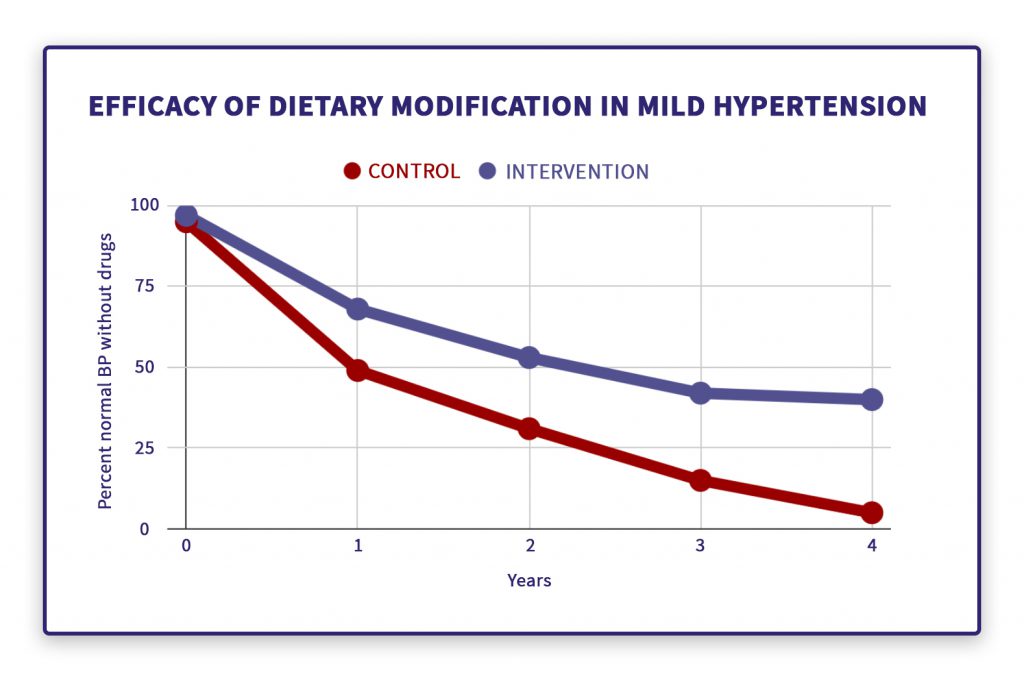 Efficacy of dietary modification in mild hypertension
Efficacy of dietary modification in mild hypertensionReproduced from:
ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 2017.
-
While physicians almost universally believe they know how to treat hypertension with medication and are quick to prescribe, there is a very poor understanding of how to collaborate with individuals to ensure medication is taken as prescribed on a sustained basis. In one 2015 study of 149 hypertensive individuals that were monitored with electronic pill boxes, 42 percent took less than 80 percent of prescribed medication. In truth, drug therapy should be used selectively, based on an in-depth diagnosis, and in moderation, with close patient-physician consultation.
-
Despite popular reports that an individual nutritional item or supplement, on its own, lowers blood pressure, this is not so. The list of individual items disproven to have a beneficial impact on blood pressure includes dark chocolate, garlic, nitrates, beets, arginine, and fish oil.
What to expect
-
While the science of how to control blood pressure, which has a direct relationship to cardiovascular risk and death, is well-understood and has improved considerably over the last 50 years, currently only half of those individuals who are both aware of and being treated for high blood pressure are “in control.” Those with high blood pressure generally have no symptoms, a strong denial reaction, and concerns about the side effects of medication. These adherence challenges mean that patient-physician collaboration is essential as further described in this chart.
Checklist for patient and physician to control blood pressure successfully- Agree on a shared goal for therapy, such as achieving a specific level of blood pressure with minimal or no side effects
- Discuss treatment options and potential decisions, including family support for those changes
-
Maintain strong patient-physician communication, through telephone calls and emails, about
- Involvement of other care providers, such as an office nurse and local pharmacist
- Side effects, challenges, and successes with therapy decisions
- Home blood pressure readings
- Any missed medication doses
- Any challenges in scheduling and attending physician office appointments
-
Ensure therapy is both affordable and simple to maintain
- Tailor daily routines to help implement the therapy, e.g., smart phone reminders
-
If using medicine as part of the therapy
- Prescribe the fewest daily doses of drugs needed and introduce one drug at a time
- Work with a pharmacist that will consolidate refills if taking multiple prescription medicines
- Look for lowest-cost alternatives, e.g., generics, preferred drugs from insurance company, pharmacist recommendations
- Use pill boxes or blister packaging
- Take medications at a routine time, e.g., first thing in the morning
- Actively identify whether changes to therapy are needed to achieve the goal and, if so, make them stepwise
-
When clinical pharmacists are included in the patient’s care team, patients experience better hypertension control. For instance, there are more medication adjustments to tailor treatment to the patient.
Citations
What is your readiness to take action, based on this information?
Reproduced from:
ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. J Am Coll Cardiol 2017.
- Agree on a shared goal for therapy, such as achieving a specific level of blood pressure with minimal or no side effects
- Discuss treatment options and potential decisions, including family support for those changes
-
Maintain strong patient-physician communication, through telephone calls and emails, about
- Involvement of other care providers, such as an office nurse and local pharmacist
- Side effects, challenges, and successes with therapy decisions
- Home blood pressure readings
- Any missed medication doses
- Any challenges in scheduling and attending physician office appointments
-
Ensure therapy is both affordable and simple to maintain
- Tailor daily routines to help implement the therapy, e.g., smart phone reminders
-
If using medicine as part of the therapy
- Prescribe the fewest daily doses of drugs needed and introduce one drug at a time
- Work with a pharmacist that will consolidate refills if taking multiple prescription medicines
- Look for lowest-cost alternatives, e.g., generics, preferred drugs from insurance company, pharmacist recommendations
- Use pill boxes or blister packaging
- Take medications at a routine time, e.g., first thing in the morning
- Actively identify whether changes to therapy are needed to achieve the goal and, if so, make them stepwise