Anemia
Anemia is a common problem seen in clinical practice and, of blood disorders, it is the most common. It is not a disease, but rather a health condition in which there are not enough healthy red blood cells to carry adequate oxygen to the body's tissues and organs. The condition may be silent, especially if there is another disease at play that is masking symptoms of anemia, and easily overlooked in its early stages. Anemia can be recent, in which case it is likely an acquired disorder, or lifelong, in which case it is likely an inherited disorder. Prevalence is consistently higher in people with low socioeconomic status, low body weight, and in females who have recently given birth.

Diagnosis
-
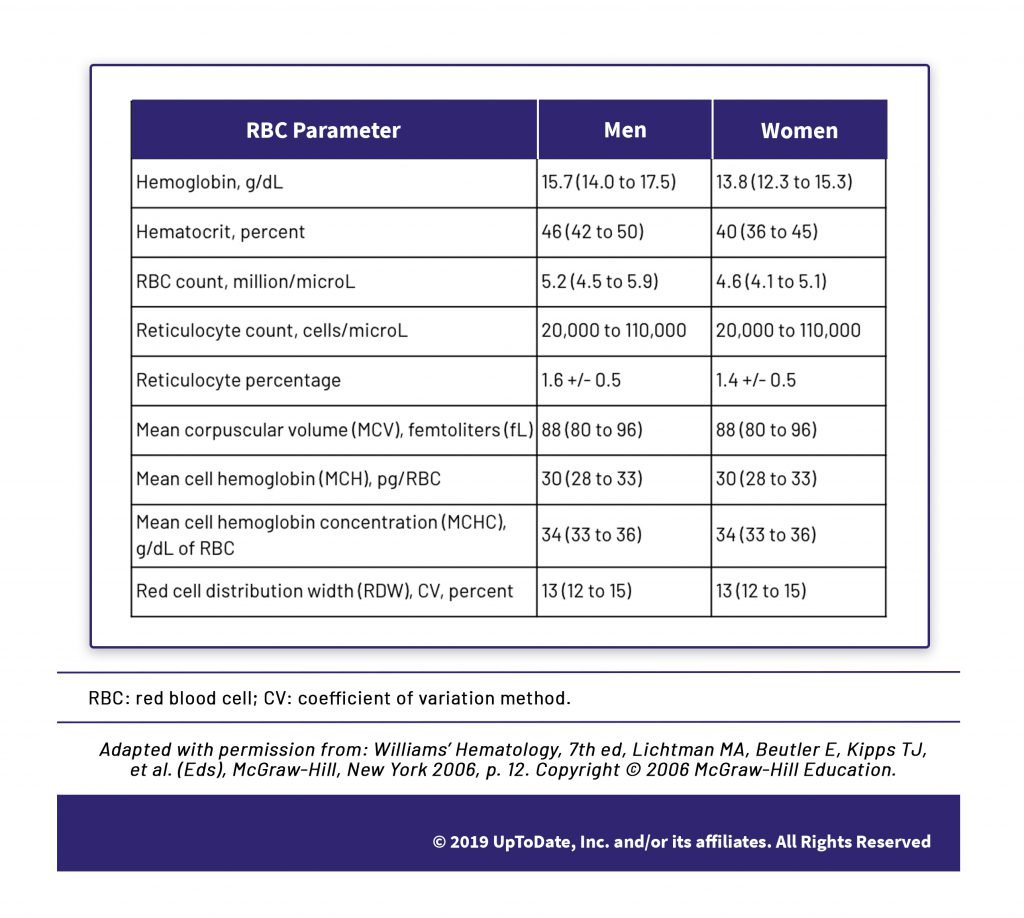
Anemia, at a designation of mild, moderate or severe, is able to be specifically and clearly defined through evaluating various red blood cell (RBC) measurements in a blood test, based on the levels outside the normal ranges shown in this chart.
-
Symptoms are the result of lowered oxygen levels, such as a persistent, but vague, feeling of exhaustion that will worsen as anemia worsens. This video shows how oxygen becomes lowered.
-
Normal RBC ranges may not apply to certain populations, such as athletes, those living at high altitude, smokers, African Americans, and those older than 65.
-
Jaundice and pallor are not as reliable indicators of anemia as was once thought due, in part, to excessively wide variation in how clinicians identify and interpret these indicators.
Causes
-
Anemia is one of the major signs of disease. It is never normal and its cause(s), even for a mild presentation, should always be sought. While the identification of anemia is straightforward, what causes anemia is may not be straightforward as there can be multiple conditions that contribute to anemia.
-
Anemia occurs if (1) bleeding causes loss of red blood cells more quickly than they can be replaced; (2) the body doesn’t make enough red blood cells; and/or (3) the body destroys red blood cells.
- Causes of blood loss, which is the most common cause of anemia, include heavy menstruation and disorders of the gastrointestinal tract.
- Causes of poor red blood cell production include lack of nutrients, such as vitamin B12 and iron, as well as bone marrow disorders.
- Causes of red blood cell destruction can include infection, autoimmune diseases, and treatment of other diseases such as cancer. The incidence and management of diseases such as cancer, heart disease, chronic kidney disease, inflammatory bowel disease, and celiac disease can prompt anemia via one of more of these three mechanisms.
-
A health history, to determine recency of symptoms, family history, and the possible influence of other diseases; a physical examination, to determine whether multiple organs are involved and gauge body condition; and laboratory testing, to determine the size, shape, and hemoglobin content of RBCs along with other confirmatory indicators such as serum iron, form an integral basis of determining the cause of anemia.
-
Despite widespread belief that anemia can be addressed with the addition of more iron in one’s diet, diet alone is not a meaningful step in preventing anemia in wealthy, resource-rich nations such as the US and Western Europe. In these countries, there is already plentiful iron content in meats and vegetables. Iron deficiency in these nations is almost certainly due to blood loss which requires the identification of a specific cause and treatment plan.
“ I Heard That…
-
Blood donation can cause anemia. Is that true?
 Yes!
Yes! Yes! And, the typical guidance offered by most blood donation centers to eat iron-rich foods is insufficient to countermand this effect. On average, women store one-third of the amount of iron as compared with men and even one instance of blood donation can fully utilize a woman’s store of iron, particularly a young woman with low body weight.
On a positive note, some people learn that their hemoglobin is low when they attempt to donate blood. However, most blood centers reassure the donor that these levels can vary from day to day and tell the donor that they should eat iron-rich foods and return to try to donate again the next day, especially if this is a first instance of low hemoglobin. This is categorically not sound medical advice. Every instance of anemia should be evaluated by a physician, and a cause for the anemia determined, before reattempting a blood donation.
And, one other note. Did you know that hospital patients can become anemic due to frequent blood draws while hospitalized? Up to 90% of patients become anemic by Day 3 in the intensive care unit. Blood tests, even in critical care settings, should be judiciously ordered.
-
I can have elective surgery even if I have anemia. Yes?
 No, that’s generally not true.
No, that’s generally not true. If anemia can be properly diagnosed and corrected, it should be addressed before proceeding with elective surgery.
Treatment
-
Since iron deficiency anemia comprises roughly half of all instances of anemia, iron replacement (delivered through a supervised medical therapy) is the most common treatment of anemia. All individuals with iron deficiency anemia should be treated and all of these treatments should be based on an identified cause of iron deficiency anemia.
-
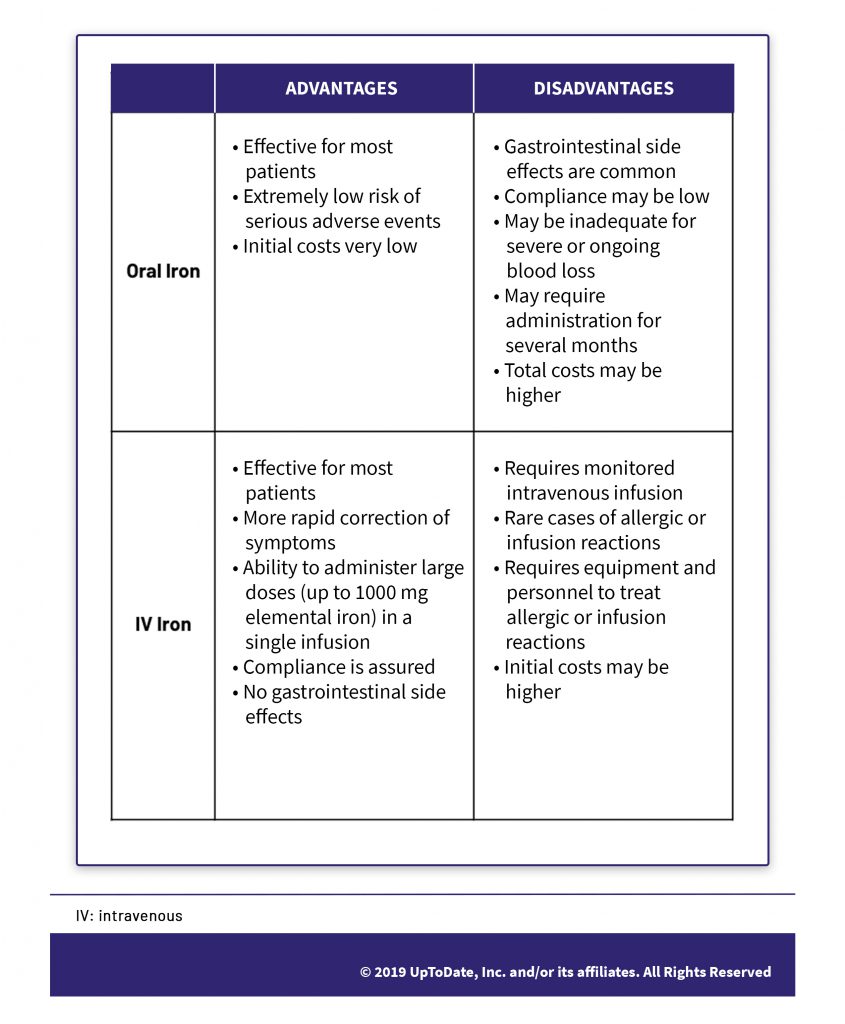
With regard to iron replacement therapies, most oral iron preparations are equally effective, in either liquid or tablet form. However, 70% of individuals experience unpleasant gastrointestinal side effects. Liquid form may be preferable as it allows for a more precise dose; other tactics such as every-other-day dosage may lessen these side effects. However, there have been substantial gains in the safety of IV iron preparations and, as shown in this chart, there are a number of common scenarios where, assuming trained personnel are available, IV administration is now recommended rather than oral iron preparations.
-
Blood transfusion can be an important step for those with severe anemia, however, a transfusion can create the risk of infection and other serious problems. There is increasing evidence that transfusions are ineffective and possibly harmful in many clinical settings in the treatment of anemia.
-
For iron replacement, despite a common view that intramuscular and transdermal administrations of iron are an easy way to address deficiency and side step unpleasant symptoms, these forms of administration are not recommended.
-
Many people commonly associate eating liver as a good way to address anemia. However, natural remedies such as eating liver – and also eating yogurt with turmeric, spinach, sesame seeds, raisins and dates as well as drinking water from a copper vessel – are not effective in the treatment of anemia.
What to expect
-
Overall, the prognosis for anemia is a good one for most people, however, this depends entirely on the cause, duration, and severity of the anemia, along with the underlying health of the individual.
-
For single-cause iron deficiency anemia where a cause has been identified and resolved and iron replacement is taken as directed, an excellent outcome can generally be expected. Iron replacement treatment, along with B12 or folate replacement if appropriate, should begin to be effective as soon as six to eight weeks and for another three to six months thereafter. A treatment may not be effective if there are conditions that prevent iron from being absorbed properly, such as celiac disease, or if there is another or alternative cause for anemia.
-
People who have had iron deficiency anemia once may be at increased risk for developing it again, depending upon why they developed anemia originally. In these people, iron supplements may be recommended to maintain the body’s iron stores. However, for most people, iron supplements and multivitamins that contain iron are not recommended as they can confound effective iron management.
Citations
- https://www.nhlbi.nih.gov/files/docs/public/blood/anemia-yg.pdf
- https://www.ncbi.nlm.nih.gov/pubmed?term=14531486
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6142528/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5479496/
- http://www.choosingwisely.org/clinician-lists/sabm-elective-surgery-in-patients-with-anemia/