Appendicitis
Appendicitis is a problem of the digestive system, specifically inflammation of the appendix due to obstruction or infection, and the most common reason for emergency surgeries. The appendix is a hollow pouch on the large intestine portion of the colon. Long thought to serve no purpose, the appendix plays a role in immune system regulation of the gut. Its importance is at its highest in fetal development and, while it diminishes in importance with age, it serves as a back-up vessel for certain “good” gut bacteria. In 2015, 345,548 Americans had appendicitis. Men have an 8.6% risk of getting appendicitis in their lifetime, while women have a 6.7% risk - but a much higher likelihood of having an appendectomy. While the incidence of appendicitis has been stable in the US and other developed economies for decades, the mortality rate, as well as the rate of appendectomies, has declined significantly.

Diagnosis
-
Abdominal, migrating pain is the most common symptom of appendicitis. Most classically, it is the first symptom to appear, starting around the belly button and then migrating to the right lower quadrant of the abdomen (where the appendix is located). Loss of appetite and/or nausea and vomiting may follow, which may then be followed by low grade fever above 99.5 degrees F. Within 24 hours after onset of pain, appendicitis will progress quickly and, in 90% of the cases, accompanied by intensifying pain, the appendix inflammation moves to acute and then gangrenous. In 20% of appendicitis cases, the appendix will perforate within the first 24 hours.
-
A diagnosis of appendicitis is determined based on two specific factors: (1) an elevated white blood cell count, through a lab test, and (2) an enlarged appendix (> 6 mm in length), through an imaging study. While a physical exam is an important step to evaluate abdominal pain, there are no physical findings, taken alone or in concern, that definitively confirm a diagnosis of appendicitis.
-
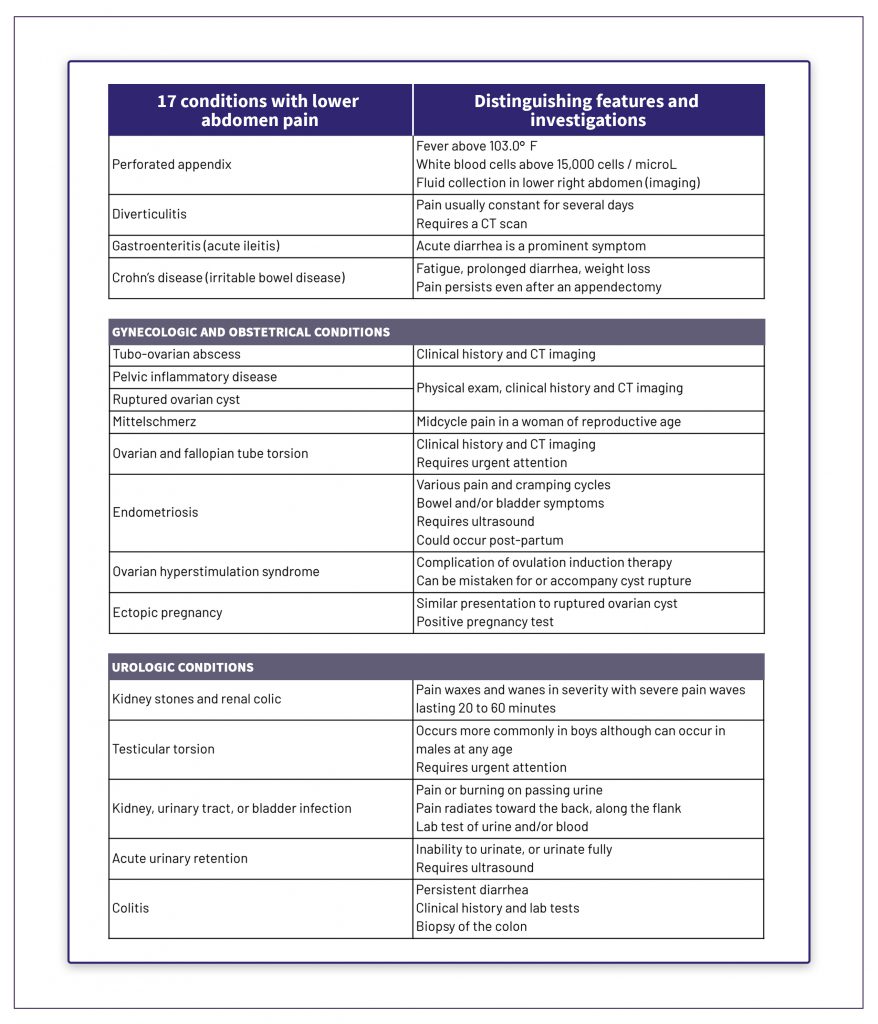
Because there are over 17 other inflammatory and infectious conditions that can mimic the signs and symptoms of appendicitis as seen in this chart, there are specific scoring algorithms to calculate the risk of appendicitis as low, intermediate or high risk. Because acute appendicitis can rapidly lead to a perforated appendix or other serious problems, even patients with low or intermediate risk of appendicitis may be admitted to hospital for close observation while lab tests, imaging, and other exams, including (rarely) surgical exploration, are performed.
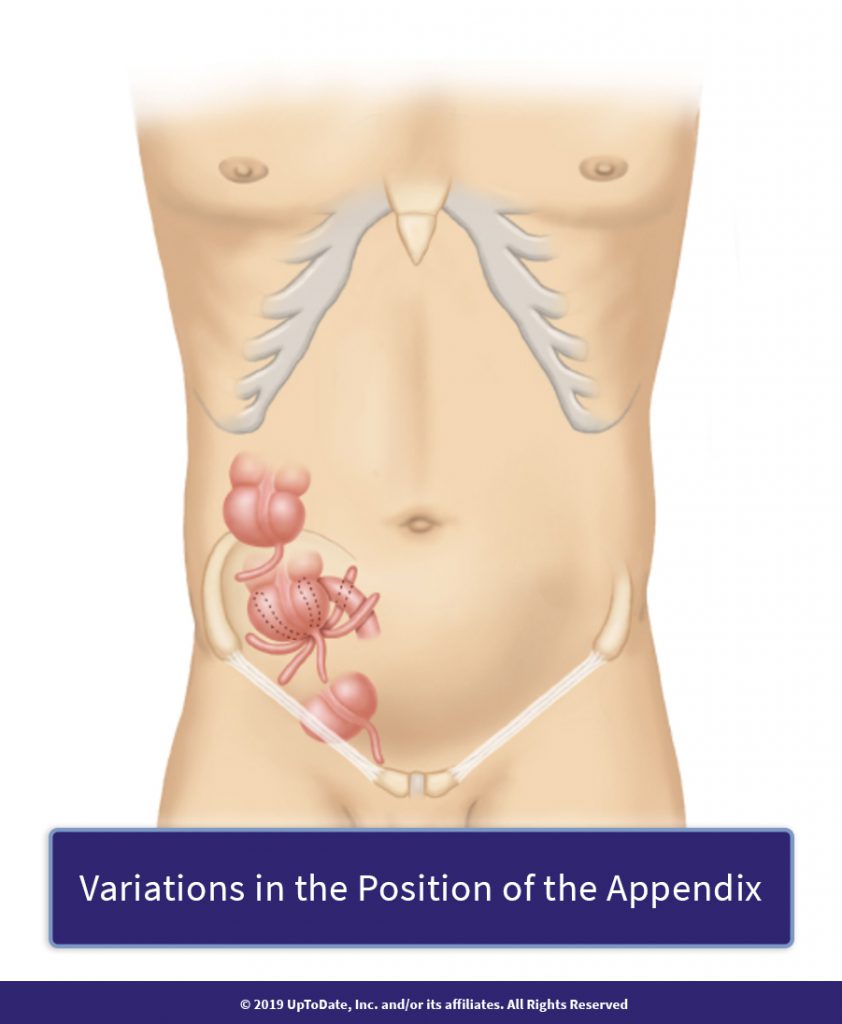 Variations in the Position of the Appendix
Variations in the Position of the AppendixBecause of normal variations in the position of the appendix, pain associated with appendicitis has a number of presentations on and around the abdomen.
-
An imaging study is a proven step to lower the rate of negative appendectomies, which is when the appendix is removed but there is no appendicitis. Women have a lifetime rate of appendectomy that is 3x higher than their rate of appendicitis, while men have a 50% higher rate.
-
Early symptoms of appendicitis can be subtle and, therefore, minimized or missed. Symptoms can be different than the classic presentation and include digestive problems and generalized malaise. Because there are normal variations in the position of the appendix, as shown in this image, pain may not migrate to the lower right quadrant of the abdomen in as many as 40-50% of those who ultimately are confirmed to have appendicitis.
-
Rectal examination, although often advocated and traditionally taught to doctors as part of the physical exam for suspected appendicitis, serves no diagnostic purpose as it does not provide a basis to rule appendicitis in or out.
Causes
-
Obstruction of the appendix is the primary cause of appendicitis. The obstruction is caused by fecaliths (hard fecal masses), calculi (like a kidney stone), an infection in the lymph nodes or another infectious process, or, in 1% of cases, benign or malignant tumors.
-
The risk of appendicitis is higher among adolescents, men, smokers, those with low fiber in their diet, those living with high air pollution, and those diagnosed with GERD.
-
The exact reason why appendicitis occurs is unclear. While there is no known genetic cause of appendicitis, family history is a risk factor based on studies of twins. Also for unknown reasons, there is a higher incidence of appendicitis in developed, rather than developing, countries and as countries become more developed, the rate of appendicitis increases.
“ I Heard That…
-
Preventive appendectomies are not a thing anymore?
 Correct!
Correct! The routine practice of removing a normal appendix to prevent future appendicitis has fallen out of practice. However, this remains a topic of some controversy. Here’s one piece that looks at the merits of an appendectomy for women who are under gynecological care and another that looks at this issue for the general population.
-
There is a connection between an appendectomy and Parkinson’s Disease?
 Actually, this is true.
Actually, this is true. Not having an appendix reduces the likelihood of Parkinson’s Disease by 20 percent. The theory, as explained in this research, is that the appendix houses certain proteins that overcome brain cells in Parkinson’s.
Treatment
-
The current standard treatment for appendicitis, as further described in this video, is laparoscopic (or “lap”) appendectomy within 12 hours of when appendicitis is diagnosed. A laparoscope is a small fiberoptic tube; it has a video camera attached to it and surgery is performed through three small incisions in the abdomen. As compared with open surgery, where an 8 to 10-inch incision is made, the advantages of lap appendectomies include inspection of other organs if there is uncertainty in the diagnosis, reduced risk of wound infection, reduced rate of negative appendectomy, less postoperative pain, shorter length of hospital stay, and quicker return to work and full function.
-
Antibiotics, initially administered intravenously, have been extensively demonstrated to be an effective non-surgical treatment for low and intermediate risk appendicitis. As compared with surgery, this course of treatment has a lower risk of complications. However, 25-40% of individuals will have a recurrence of appendicitis and require surgery within 1 to 5 years. For this reason, antibiotics are currently used as an alternative to surgery only with individuals who refuse surgery or are considered high risk candidates for surgery.
-
If the appendix perforates before surgery, treatment may involve antibiotic management for several days before an appendectomy.
-
Given the high rate of negative appendectomies, an important decision – to discuss before surgery – is whether to remove the appendix if it appears to be normal during an intended appendectomy. The evidence of whether to remove a normal appendix is contradictory and, therefore, this practice is highly specific to the preferences and situation of the individual and his or her surgeon.
-
As more is learned about the recurrence of appendicitis, including for whom that is most likely and why, antibiotics may become a more widely used alternative to surgery.
What to expect
-
While surgical complications are always possible, full recovery is the normal expectation. Individuals are discharged from hospital following surgery once pain is limited, fluid intake is good and there is no vomiting. In fact, same-day discharge is an increasing trend with lap appendectomies.
-
Complications include whether the appendix has become perforated, which occurs in 13 to 20 percent of individuals with appendicitis, and at a higher rate for men and for older adults. The perforation can be localized, and therefore lower risk, or “free,” in which there is a higher risk of more serious problems such as sepsis. Individuals with a perforated appendix are also at higher risk of surgical site infection and hospital readmission. However, the management of a perforation is well-understood and, while serious, the expectation for those individuals without other health problems is also for full recovery.
Citations
- For an understanding of incidence and prevalence of appendicitis:https://journals.lww.com/annalsofsurgery/Fulltext/2017/08000/The_Global_Incidence_of_Appendicitis__A_Systematic.8.aspx
- For a thorough review of diagnosing and treating acute appendicitis:https://www.wses.org.uk/wp-content/uploads/2018/07/acute-appendicitis-guidelines.pdf
- To learn about the outcomes of laparoscopic appendectomy:https://www.ncbi.nlm.nih.gov/pubmed?term=21173695
What is your readiness to take action, based on this information?
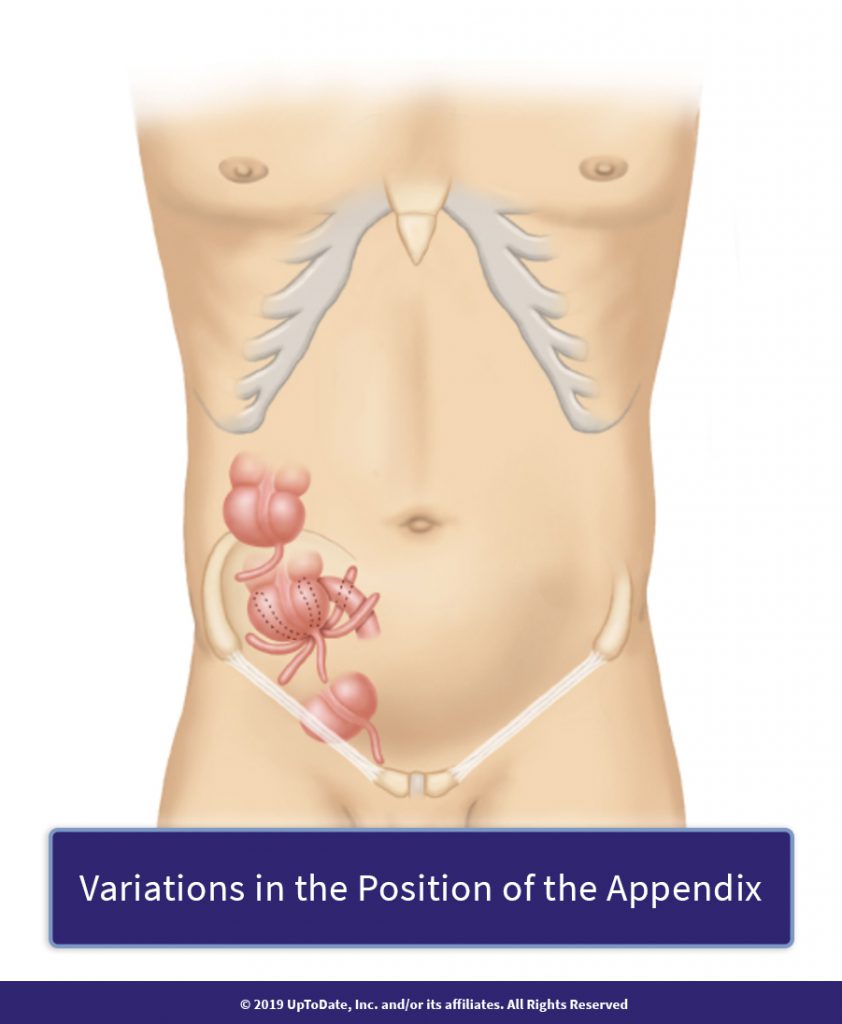
Because of normal variations in the position of the appendix, pain associated with appendicitis has a number of presentations on and around the abdomen.