COVID-19
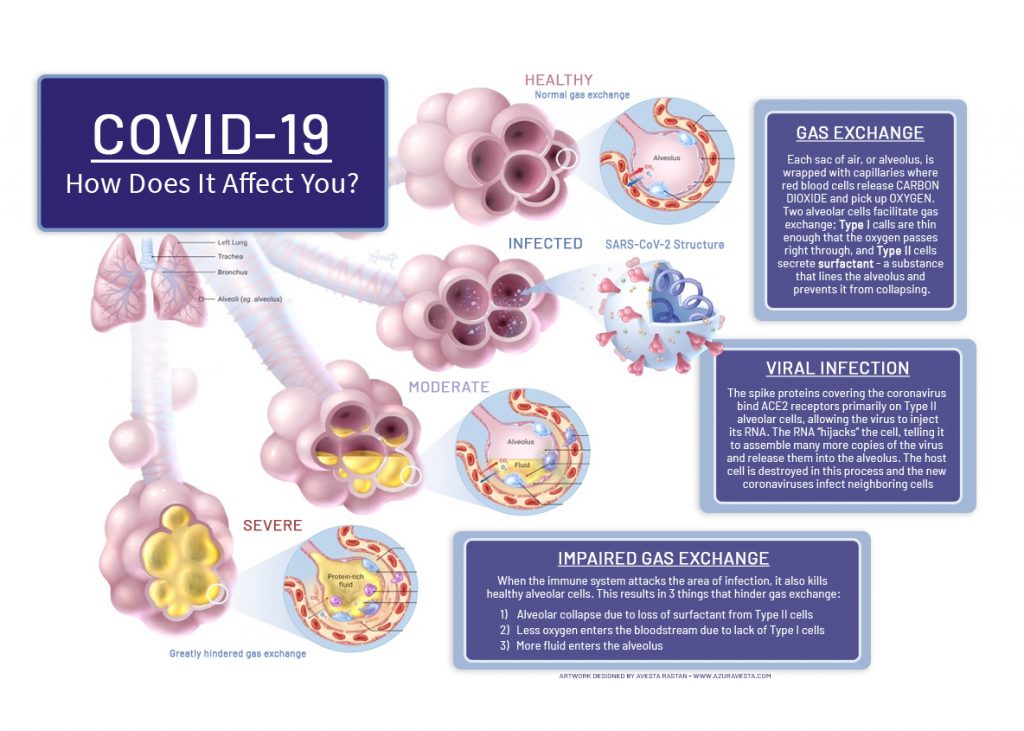
COVID-19, short for “coronavirus disease 2019,” is an infectious disease that mainly affects the lungs, specifically those cells that keep lungs fluid, clean, and infection free. While the coronavirus family is a longstanding cause of colds and other upper respiratory infections, this particular virus is novel yet genetically similar to the severe acute respiratory syndrome (SARS) virus. Because testing capacity for COVID-19 is low in most countries, prevalence is uncertain. The most stable, real-time indicator of prevalence, and comparator across time and location, is the rate of hospital admissions for COVID-19, which is currently more than 50 per 100,000 people in the United States. The outbreak has been so rapid and in so many countries that COVID-19 is currently described as a pandemic.

Diagnosis
-
Among a large population with normal distribution of age and underlying health conditions, the impact of COVID-19 can create a wide range of impact as depicted in this chart.
- 81% of confirmed COVID-19 cases are mild (ranging from no symptoms to mild pneumonia);
- 14% are severe (with breathing impairment or >50% lung involvement on imaging); and
- 5% are critical (respiratory distress, failure of other organs).
-
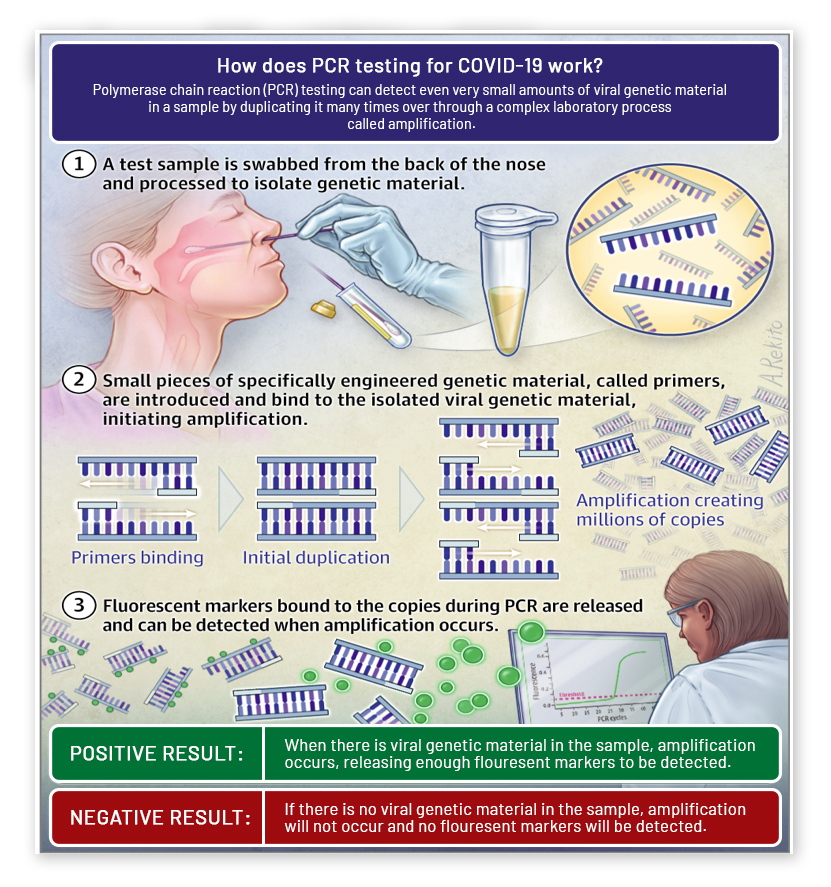
A diagnosis of COVID-19 is definitively made with a laboratory “PCR” test, as shown in this picture. There are false negatives during early onset, due to poor sample collection, and during the recovery phase. A chest X-ray can be an important means of ruling COVID-19 in and out, as well as a flu test.
-
A sudden onset of fever and respiratory tract symptoms (such as dry cough and shortness of breath) is reason to suspect COVID-19. A severe lower respiratory tract illness that does not have any other clear cause is also a reason. Along with tiredness, these symptoms are present in the great majority of COVID-19 cases. Using a pulse oximeter, at home, is an important step in evaluating breathing difficulties; a reading below 95, taken from a warm digit (finger), is reason for an in-person medical evaluation.
-
Problems with the sense of smell (known as anosmia), which can also interrupt the sense of taste, have been reported as common symptoms in patients with COVID-19, based on small studies in Italy, Germany, and South Korea. The American Academy of Otolaryngology-Head and Neck Surgery reports that anecdotal evidence is “rapidly accumulating” that a smelling disorder is a significant symptom associated with COVID-19, although not as common as fever and lower respiratory tract symptoms and not on its own.
-
Certain presentations of COVID-19 do not fit the emerging symptom profile. For instance, gastrointestinal symptoms, such as nausea and diarrhea, or upper respiratory problems may be the presenting symptoms of COVID-19. Some patients do not present with fever. An additional potential symptom is emerging and is under investigation by researchers including the International Federation of Podiatrists: purple-colored lesions, such as those of chickenpox, measles, or chilblains, that appear around the toes.
-
Despite popular belief, identifying COVID-19 by holding your breath for 10 seconds or more without coughing or feeling discomfort is not a way to identify a COVID-19 infection.
Causes
-
While we do not fully understand the route of transmission of COVID-19, the main mode is respiratory droplets that move from “person-to-person” as shown here. Therefore, the cause of COVID-19 can be understood as enabling droplet-based person-to-person transmission, by:
- Poor hand-washing habits in terms of frequency and/or completeness.
- Frequently touching one’s eyes, nose, or mouth with one’s hands. Note that if wearing a cloth mask, scarf, bandana, glasses or gloves helps an individual not touch their eyes, nose or mouth, they should wear a routinely cleansed cloth mask, scarf, bandana, glasses, or gloves.
- No or limited disinfection of surfaces, especially plastic or stainless steel, that are commonly touched.
Primary Method of COVID-19 Transmission- One person who has COVID-19 (whether symptomatic or not) creates droplets with active virus particles by sneezing or coughing or talking
- These droplets travel, up to distances of 6 feet in practical terms, through the air before falling
- These droplets land in another person’s mucous membranes (i.e., their eyes, nose or mouth) or elsewhere on that person or a surface
- And that person inhales the droplets; or touches the surface where the droplets landed and then touches his or her eyes, nose, or mouth
-
While COVID-19 is highly infectious for everyone since this is a new virus in humans, the risk of serious infection is increased:
- With age. The majority of individuals hospitalized with COVID-19 are, as shown in this chart, older, with a median age of more than 45 years old.
- When certain underlying health conditions exist. COPD increases the odds of a more serious infection by 5x, cerebrovascular disease by 3x, chronic kidney disease by 3x, cardiovascular disease by 2x, hypertension by 1.5x, and diabetes by 1.25x odds. Of note, these odds are not adjusted for whether that underlying health condition is severe or mild nor are they adjusted for the presence of other risk factors, such as advanced age or smoking.
- With smoking, which carries the same level of increased risk as COPD but is a reversible risk for those that quit smoking. Vaping is also believed to be a risk factor, however, is not quantified.
- For men.
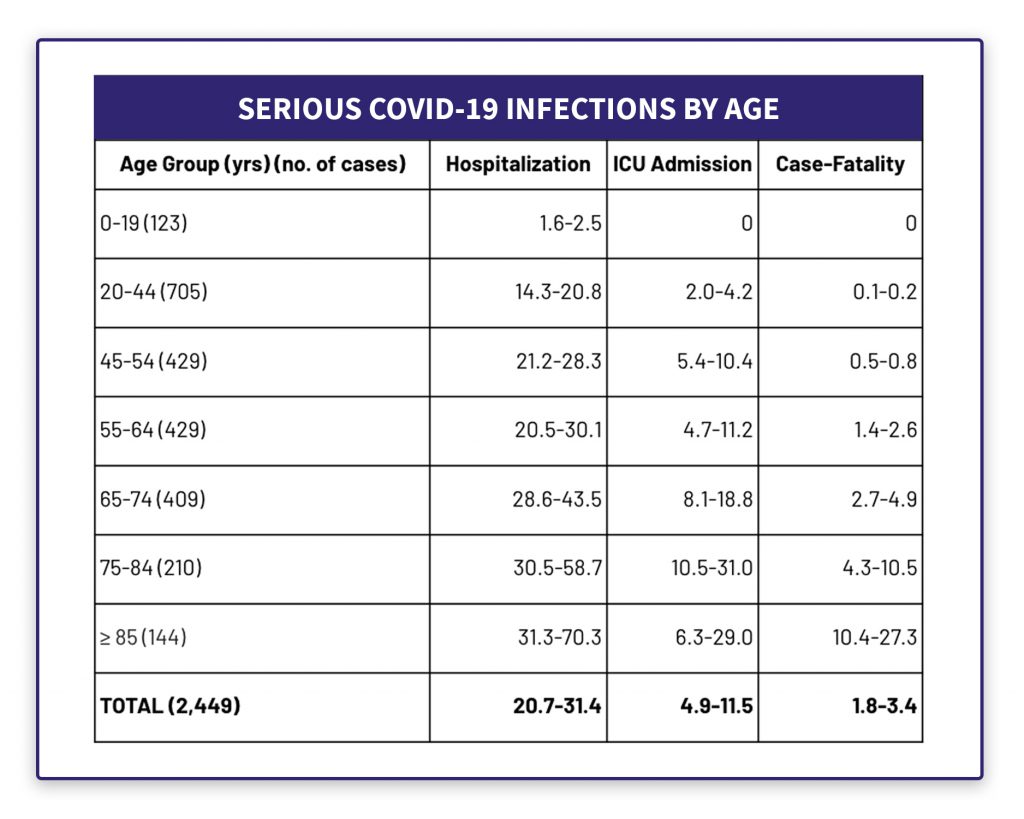 Rate of Serious COVID-19 Infections
Rate of Serious COVID-19 InfectionsAs reported by the Centers for Disease Control and Prevention, based on US hospital admissions from February 12 – March 16, 2020
-
The period of infectivity is thought to be 14 days, however, this timeframe is not certain. Key questions include the degree of infectiousness:
- During the period of onset with symptomatic COVID-19;
- After symptoms subside during recovery; and
- Of those with asymptomatic COVID-19.
-
Coronaviruses, based on a study by the National Institute of Allergy and Infectious Diseases, can remain in the air for several hours. It is uncertain whether these aerosols, which are smaller droplets that are emitted when people breathe and speak, are a meaningful mode of COVID-19 transmission, particularly once they evaporate. Further, airborne transmission is an atypical mode of transmission for coronaviruses.
-
With regard to food preparation, coronavirus strains could be present at low and freezing temperatures for a certain period, however, basic food hygiene and safety practices should prevent transmission of the virus through food.
-
There is some mild evidence that those individuals with blood group type A have a higher rate of COVID-19 infection than those with blood group type O.
-
There is no evidence, despite some speculation, that the route of COVID-19 transmission is
- Through mosquitoes or other insects
- Through drinking water
- Through domesticated animals, such as dogs or cats
- Through blood products or needle sticks
- Changed by climate, either temperature or moisture level or sunlight
“ I Heard That…
-
A wearable device can identify a possible COVID-19 infection?
 Yes!
Yes! In fact, there’s enough merit to the performance of at least one wearable that an investigation is underway. Check out the research announced by West Virginia University Rockefeller Neuroscience Institute, WVU Medicine, and smart ring maker Oura Health in which smart rings are being distributed to critical care providers in a number of health systems. Don’t have or want an Oura ring? Consider buying an inexpensive pulse oximeter as a means of keeping track of your lung health.
-
There are a lot of new testing locations for COVID-19.
 Indeed.
Indeed. Check out this database to identify a testing site near you from among over 1,000 COVID-19 locations, if you and your doctor decide a test is appropriate. And, if you test positive, please consider being a beta tester for a new contact tracing app by writing to chris@brasstacksapps.com. Speaking of contact tracing, all of us can use this tool, built by a group at Boston Children’s Hospital and Harvard, which does not collect IP addresses or otherwise track individual users.
-
I should get a flu shot. Is that true?
 You haven't gotten one this year yet? Yes!
You haven't gotten one this year yet? Yes! Getting an annual flu shot does nothing to lower your risk of becoming infected with COVID-19. However, now is an excellent time to limit your risk of becoming infected with seasonal flu, noting that the 2019-2020 influenza season in the US has been moderately severe to date. And, talk with your doctor about whether you are a good candidate for the pneumonia and shingles vaccines. Finally, make sure you are up-to-date with all other routine vaccinations, such as measles, mumps, and rubella.
Treatment
-
A number of approaches are being investigated to treat COVID-19, however, there is currently no treatment for COVID-19. Of note, the virus itself is well-defined, with the entire DNA sequence laid out for researchers. Over 1,300 clinical trials are underway worldwide and, whenever possible, should be considered; a registry of international clinical trials can be found at clinicaltrials.gov.
-
Among others, there are 4 primary treatment paths that are under active investigation, however, with limited valid data about efficacy, optimal use, side effects and toxicity.
- Remdesivir, an experimental antiviral, with strong promise;
- Convalescent blood plasma, subject to logistical limitations, approved by the FDA for emergency use and derived from those individuals that are recovered from COVID-19 that have antibodies that attack the COVID-19 virus;
- Chloroquine and, a new version, Hydroxychloroquine, a drug used to treat malaria, lupus and arthritis and also approved by the FDA for emergency use; and
- Interleukin-6 pathway inhibitors, an anti-inflammatory used for management of diseases like rheumatoid arthritis.
-
Current protocols reflect a very wide range of experience about how to best provide respiratory support for those individuals that are severely infected, ranging from breathing therapies (like ironing) to use of respirators. At least six academic medical institutions, specifically Brigham and Women’s Hospital, Massachusetts General Hospital, Michigan Medicine, Nebraska Medicine, Penn Medicine, and University of Washington Medicine, have developed publicly available COVID-19 management protocols based on field experience.
-
Use of acetaminophen is preferred for symptom management with COVID-19 if possible; NSAIDs have been theorized to cause harm in patients with COVID-19, however, these concerns were raised with anecdotal data and there is limited evidence this is so.
-
Despite widespread reports, there is no evidence that gargling with saline or other substances, nor rinsing nasal passages with saline, will protect people from becoming infected with the novel coronavirus. That said, these are techniques to ease cough and cold symptoms.
What to expect
-
The median time between infection and symptom onset has been estimated as 5.1 days. Within another 7 days, mild infections resolve while more severe infections become worse, potentially requiring hospitalization. A serious infection can last a month or more; symptoms can ease and then return with even more vigor. This video further describes the wide range of potential scenarios for both individuals and the population as a whole.
-
Whether someone who has been infected with COVID-19 and recovers can become infected again depends on an antibody analysis that is only now seriously underway. While antibodies to the virus are induced in those who have become infected, it is unclear if those antibodies are protective for all individuals and, if so, how long any protective effect will last.
Citations
- For more about prevalence of COVID-19, including issues and challenges with commonly reported data:https://www.thelancet.com/journals/lanres/article/PIIS2213-2600(20)30162-4/fulltext
- For more about how coronaviruses, including COVID-19, cause impact:https://www.scientificamerican.com/article/how-coronaviruses-cause-infection-from-colds-to-deadly-pneumonia1/
- For more about how other health issues, and which health issues, increase the risk of a serious COVID-19 infection:https://www.ncbi.nlm.nih.gov/pubmed/32267833
- For more about treatment and management of COVID-19, especially for those with a severe illness:https://www.idsociety.org/practice-guideline/covid-19-guideline-treatment-and-management/
- And more here about the studies and trials underway to identify treatments of COVID-19:https://jamanetwork.com/journals/jama/fullarticle/2764727
What is your readiness to take action, based on this information?
- One person who has COVID-19 (whether symptomatic or not) creates droplets with active virus particles by sneezing or coughing or talking
- These droplets travel, up to distances of 6 feet in practical terms, through the air before falling
- These droplets land in another person’s mucous membranes (i.e., their eyes, nose or mouth) or elsewhere on that person or a surface
- And that person inhales the droplets; or touches the surface where the droplets landed and then touches his or her eyes, nose, or mouth
As reported by the Centers for Disease Control and Prevention, based on US hospital admissions from February 12 – March 16, 2020