Pediatric ADHD
Attention deficit hyperactivity disorder (ADHD) affects brain development and activity, is one of the most common problems of childhood, first occurs in early childhood, and persists an average of 7 years. There are two core categories of traits, one is hyperactive-impulsivity and the other is inattention, each with its own pattern and course of development and, most commonly, combined with one other. ADHD is considered a chronic disease as well as a disability under the Individuals with Disabilities Education Act. The prevalence of ADHD spans from 9 to 15% among school age children, based on studies in many countries including the US.

Diagnosis
-
Since hyperactive-impulsivity and inattentiveness occur to some extent in all children, it is the particular combination of persistence, pervasiveness, and functional complications of these behaviors that lead to a diagnosis of ADHD. A proper diagnosis is guided by the consensus criteria of the American Psychiatric Association, most recently updated in 2013.
-
ADHD is more than 2 times as prevalent in boys as compared with girls, as show in this chart. Prevalence is increasing for both genders over time, across many countries including the US, potentially based on increasing awareness.
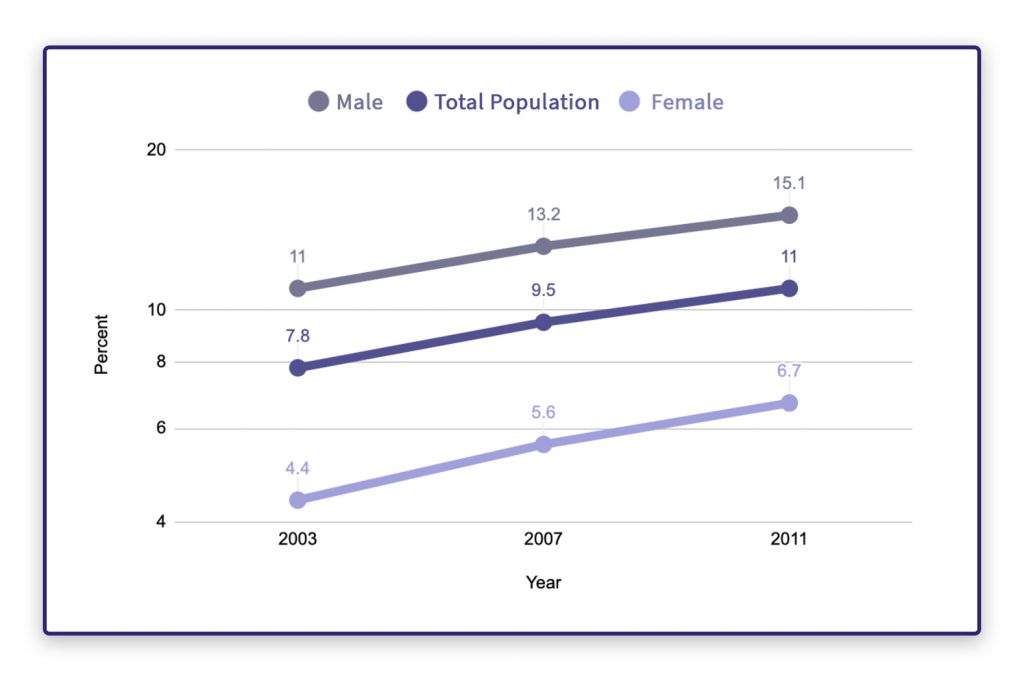 Trends in Prevalence of Children Ever-Diagnosed with ADHD
Trends in Prevalence of Children Ever-Diagnosed with ADHDData from National Survey of Children’s Health (NSCH)
-
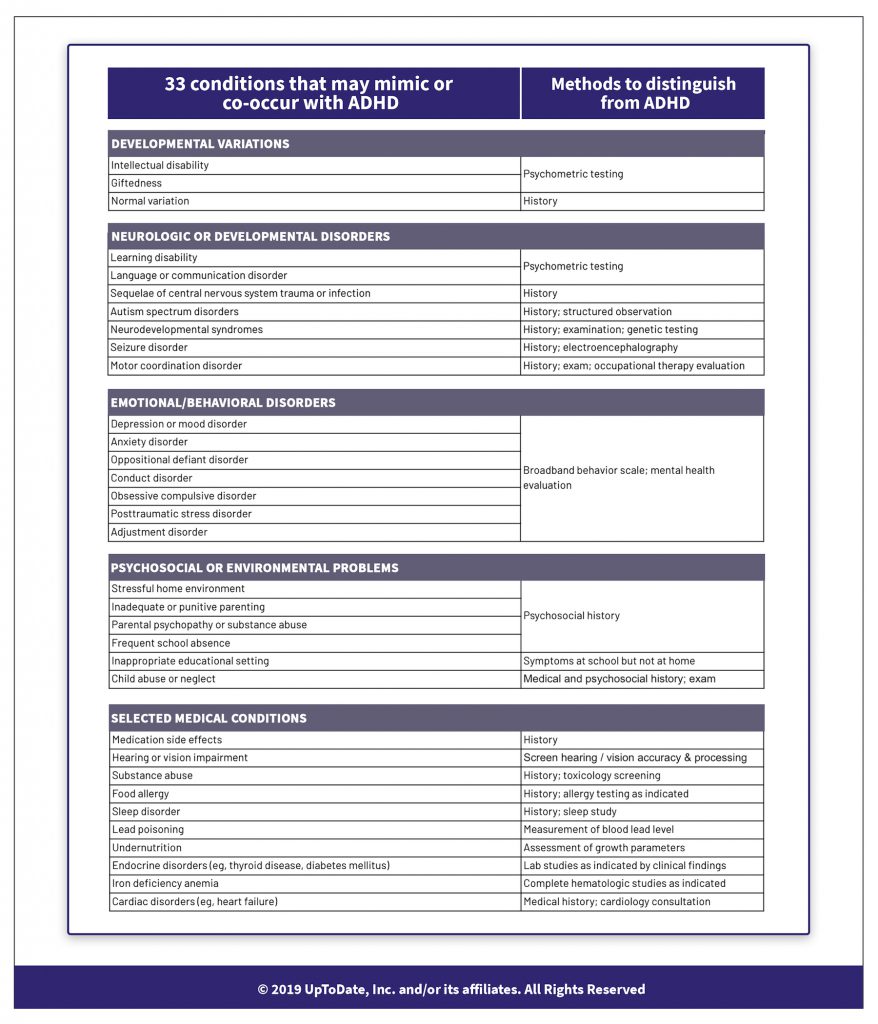
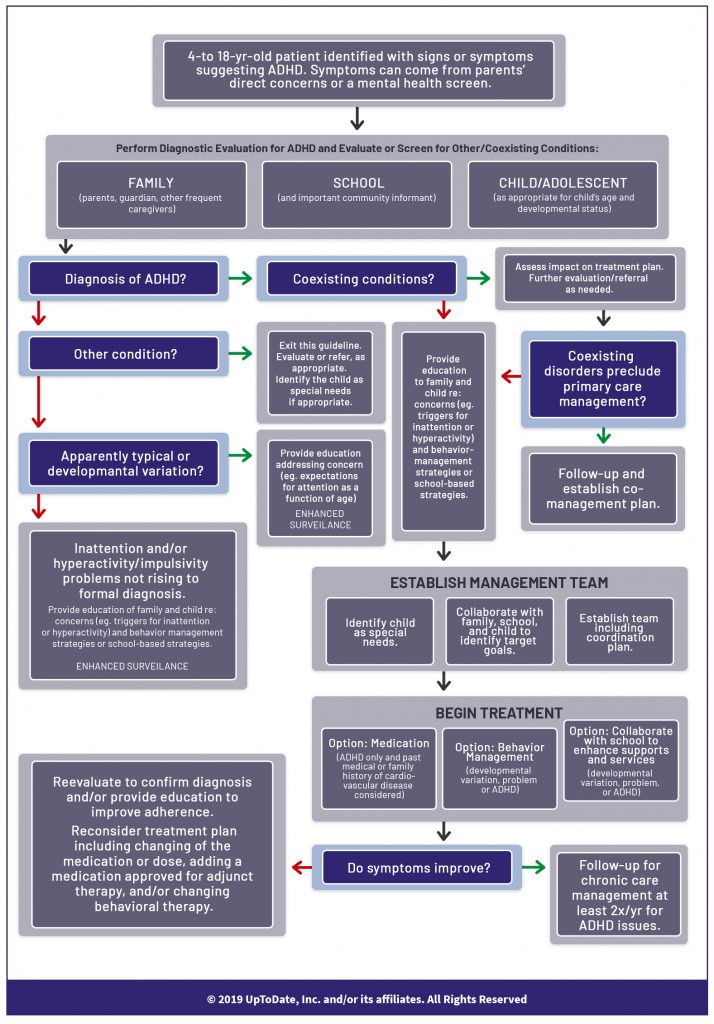
A diagnosis of ADHD requires that other physical, situational, or mental health conditions that could account for the symptoms are accounted for. The symptoms of ADHD overlap with over 33 individually described medical conditions, including visual processing, auditory processing, developmental variations such as giftedness or coordination disorders, and sleep problems. Further, as many as one-third of children with ADHD have a concurrent health issue. Quite a thorough evaluation, involving more than one care provider, is required to confirm a diagnosis of ADHD and related issues, as summarized this chart.
-
There is a widespread belief that ADHD medications (typically stimulants), if they work to improve a child’s behavior, serve to confirm a diagnosis of ADHD. This is not true. Studies have shown that stimulant medications can make nonspecific improvements in a child’s behavior whether that child has ADHD or not. Further, this approach can be harmful as it may mask non-ADHD problems, delay the use of ADHD-focused interventions, and/or introduce unnecessary side effects of ADHD medicines.
-
A quantitative EEG is approved by the US Food and Drug Administration for assessment of children for ADHD, however, it has been determined not to be a reliable basis of ADHD diagnosis.
Causes
-
Genetics appears to be a primary factor in the cause of ADHD, which manifests itself as low levels of dopamine in the brain, based on studies of twins, family-based and case-control studies, and population-based genetic testing. These causes, and a broader overview of ADHD, are further described in this video.
-
Various environmental factors may play a secondary, however controversial, role due to a large number of studies with either mild, conflicting, or non-causal findings. These factors include dietary influences, such as food additives, deficiencies in fatty acids, iron and zinc; prenatal influences, such as medications, alcohol tobacco smoke, lead exposure, and pre-maturity; and head trauma in young children.
-
Despite popular belief, research does not support the premise that ADHD is caused by eating too much sugar, watching too much television, poor parenting, or poverty.
“ I Heard That…
-
But my child didn't. When I write it down, all is well. Is that ADHD?
 Not necessarily.
Not necessarily. Another possibility is auditory processing disorder, which is estimated to impact roughly 5% of children and has symptoms that are virtually identical to ADHD. And, a different pattern of response by a child to visual directions as compared with verbal directions could be an important signal. Scientists argue here in a sharply worded piece that auditory processing disorder is a well-established and identifiable disorder that needs far greater attention.
-
Brain games are still a thing?
 Yes, actually.
Yes, actually. But not everyone agrees. Two large groups of researchers studied the exact same data and came to exactly opposite conclusions about the impact of brain games on neurological conditions like ADHD. There are good arguments on both sides; see for yourself here.
Hot off the press, Akili is rolling out a video game, initially for free, to be used by, and pending FDA approval, prescribed to children with ADHD. The approach of using “software treatment” to “actively reduce severity of ADHD” is backed-up by quite a rigorous randomized control trial (RCT) as described here.
Treatment
-
The general principles of treatment involve coordination of care through a disciplined set of decisions, involvement of parents and teachers, setting target goals, treating relevant concurrent health issues, and involving other care providers as further described on this flow chart. The kinds of medical professionals that could be involved include, in addition to a pediatrician, include an occupational health therapist, audiologist, optometrist, developmental behavior pediatrician, and educational psychologist.
-
Behavior therapy and, with careful management and for children older than 6, medication are the time-tested approaches to ADHD, with increasing evidence that a combination of the two is the most effective approach.
-
The Centers for Disease Control and Prevention also recommends training for parents and in the classroom which, the evidence indicates, creates improvement as long as the training is consistently implemented. Other treatment approaches, including social skills training, sleep training, daily physical activity, and mindfulness training, are possibly beneficial but not consistently proven to be so.
-
Popular press aside, there is no evidence that dietary changes, such as elimination diets and essential fatty acid supplements, are recommendable treatments for ADHD. Other alternative therapies promoted as cure-alls for ADHD, including megavitamins, herbal and mineral supplements, and chelation, are not only not recommendable but can cause serious other problems in children.
What to expect
-
How ADHD will manifest itself over time is uncertain as this is a relatively newly described medical condition that has been studied intermittently over the last 20-30 years. For public health purposes, ADHD is not a reportable disease. Based on what is known, the outlook appears to depend on the severity of symptoms at onset, whether other related health issues also exist, intellect, social advantage, and the degree to which the condition responds in the immediate-term to treatment. Some children’s brains develop such that all symptoms dissipate by adolescence. Early and effective management of ADHD may be helpful in improving adult outcomes.
-
Issues to be concerned about as children grow up with ADHD include a potential higher rate of injury and self-injury, vehicle driving safety, academic functioning, and substance abuse.
Citations
- For a recent and full history of pediatric ADHD management:https://www.ncbi.nlm.nih.gov/pubmed?term=31570648
- For a series of targeted updates about management of pediatric ADHD:https://effectivehealthcare.ahrq.gov/products/adhd-update/systematic-review-2018
- For more about the causes of ADHD:https://www.ncbi.nlm.nih.gov/pubmed?term=17718779
- For more about medications to treat ADHD:https://www.sciencedaily.com/releases/2018/08/180807192845.htm
- And, finally, a thorough set of vetted resources and tools:https://www.nichq.org/resources?search=adhd
What is your readiness to take action, based on this information?
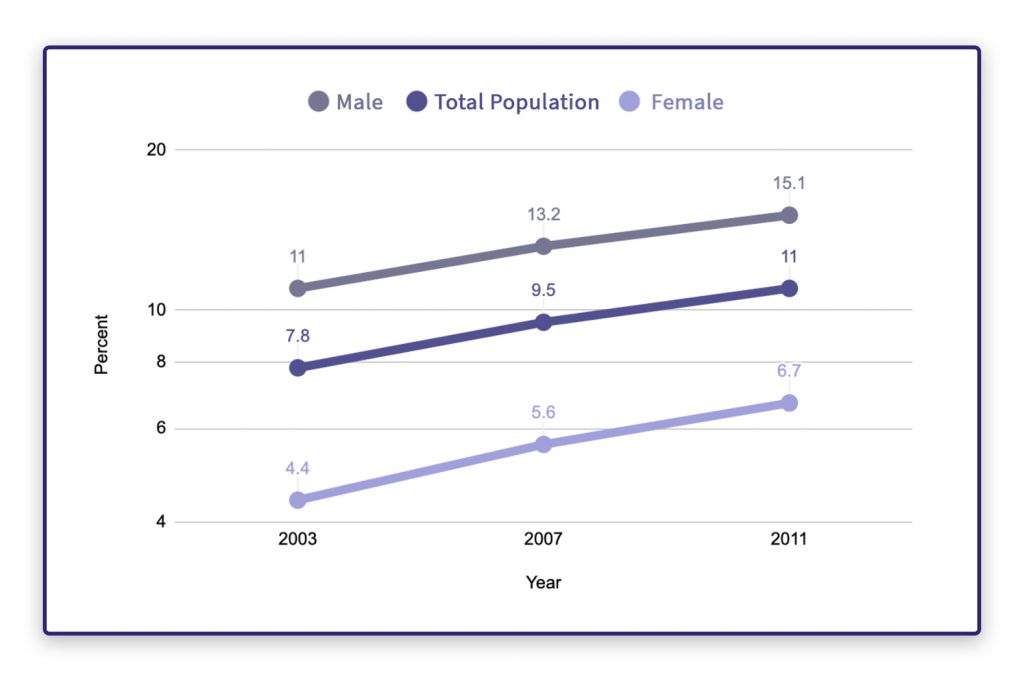
Data from National Survey of Children’s Health (NSCH)